Cystic Fibrosis (CF) is an inherited disease, typically affecting the lungs, pancreas, liver, skin, and urogenital tract due to mutations in the cystic fibrosis transmembrane conductance regulator (CFTR) gene. It follows an autosomal recessive pattern, impacting a patient’s life expectancy, which commonly averages around 33 years. The disease significantly affects the quality of life, necessitating rigorous treatments such as daily chest physiotherapy, frequent use of inhaled medications, oxygen therapies, recurrent intravenous antibiotic treatments, and nutritional support.
However, advancements in treatments and enhanced disease management strategies have notably increased the life expectancy of recently diagnosed newborns to approximately 50 years of age.
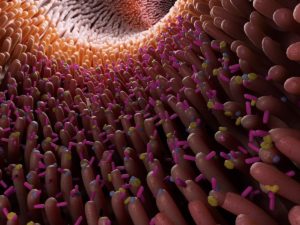
The CFTR gene encodes an anion channel responsible for regulating the transport of chloride and bicarbonate ions across cell membranes. Mutations in this gene disrupt the normal flow of epithelial lining fluid, particularly in the lungs and pancreas. This disruption causes the formation of thickened mucus in the airways, leading to frequent respiratory infections, and pancreatic insufficiency contributing to malnutrition and diabetes.
Over 2100 mutations have been identified in the CFTR gene, categorized from I to VI based on their impact on the CFTR protein. The most common mutation, F508del, falls under class II mutations characterized by processing and trafficking defects. Other classes lead to varying levels of protein activity, from complete absence to residual function.
The introduction of systematic newborn screening across numerous European countries has been pivotal in improving CF prognoses. This screening involves a simple blood test to identify CFTR mutations in infants, followed by parental genetic analysis for preconceptional or prenatal counseling and familial investigation.
The development of two types of molecules—potentiators, enhancing CFTR function at the cell surface, and correctors, aiding CFTR transport to the cell surface—has revolutionized CF treatment. Early screening facilitates timely access to modulator therapies, now administered from the age of 4 months.
Ivacaftor, a CFTR potentiator designed to improve gating defects, has been demonstrated in several clinical trials involving children to augment lung functions, reduce risk of pulmonary exacerbation, improve patient’s quality of life and help weight gain. For patients having at least one F508del allele severely reducing protein levels at the epithelial membrane, biterapy combining a CFTR potentiator and a corrector is essential. The combination of ivacaftor with the tezafactor corrector, named Symkevi therapy, significantly improves lung function and is generally safe and well tolerated. Finally, a new corrector named elexacaftor was proven effective to increase the amount of mature CFTR protein and CFTR activity when taken in combination with tezafactor and ivacaftor. The combination named Kaftrio has greatly improved the prognosis and quality of life of patients involved in clinical trials by reducing the need for daily care. However, long-term studies have to confirm these findings. The triple therapy has been approved by the European Medicines Agency in August 2020 and is today available in many European countries including Switzerland for its use in children aged 6-11 years.
In summary, advancements in CF treatment, particularly the development of personalized therapies targeting CFTR gene mutations, have significantly improved patient outcomes. These tailored treatments, such as Kaftrio therapy, have notably enhanced quality of life and life expectancy for many individuals with CF. However, challenges persist for around 2100 patients who cannot benefit from these therapies due to various reasons, including ineligibility or absence of specific mutations.
In Switzerland, the Téléthon Foundation fights against rare genetic diseases including CF by financing research at universities and hospitals, educating caregivers, increasing awareness about these diseases, and supporting patients in their daily lives.
We at 4Bases are proud to contribute to this battle by offering the CFTR panel, a CE-IVD kit to profile hereditary variants in Cystic Fibrosis. We are convinced that diagnosis is a key step in combating CF!
Source: Foucaud, P., & Mercier, J. (2023). CFTR Pharmacological Modulators : a great advance in cystic fibrosis management. Archives de Pédiatrie, 30(1), 1‑9. https://doi.org/10.1016/j.arcped.2022.11.019