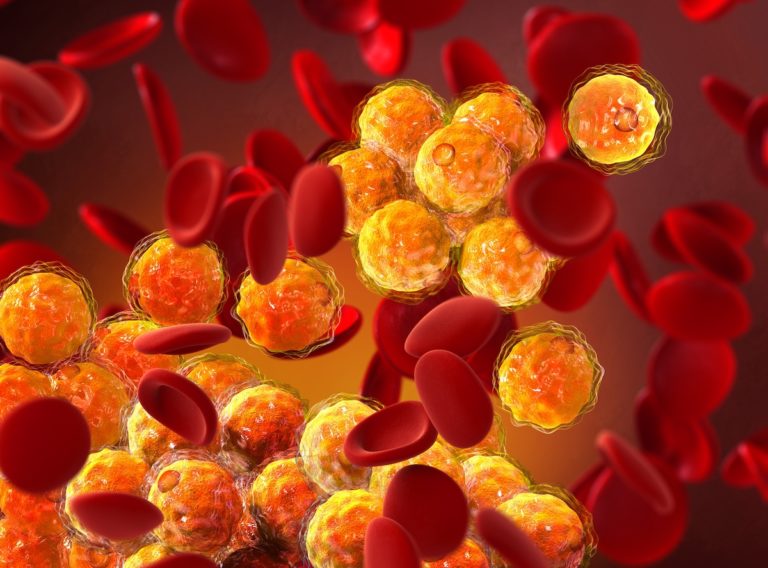
Familial hypercholesterolemia (FH) is a genetically inherited disease characterized by high blood levels of total cholesterol and LDL cholesterol (Low-Density Lipoprotein, often referred to as “bad cholesterol”). Homozygous FH is rare, with a prevalence of 1:160-400’000, but heterozygous FH presents a prevalence of 1:313 and increases the risk of developing a premature coronary vascular disease by about 20 folds1. Following typical signs such as high LDL blood-levels, family history of early heart attack or heart disease, or swollen or pain in Achilles tendons, genetic testing is a key step to confirm FH diagnosis.
Treatments aim at reducing cholesterol concentration to a healthy level. Statins, or HMG-CoA (hydroxymethyl glutaryl coenzyme A reductase) inhibitors, are the most commonly used treatments. They inhibit or lower the production of cholesterol by blocking the critical step of cholesterol synthesis2. However, statins present individuals variation in response to the treatment which can be predicted by polygenic SNPs (Single Nucleotide Polymorphism) identification.
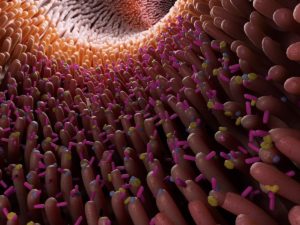
FH is caused by pathogenic variants in the LDLR (low-density lipoprotein receptor), APOB (apolipoprotein B), or PCSK9 (proprotein convertase subtilisin/kexin type 9) genes. In 10% of cases, FH is due to CNVs (Copy Number Variants, structural variations in the genome that involve the duplication or deletion of a segment of DNA with a size larger than 50 base pairs) in LDLR. Indeed, the LDLR gene is located on chromosome 19, the chromosome containing the highest percentage of Alu repeats which are the most common transposable elements in the human genome. The LDLR gene contains 98 Alu repeats resulting in whole exons deletions. MLPA (multiplex ligation-dependent probe amplification) is the gold-standard method to detect CNVs. This multiplex PCR (Polymerase Chain Reaction) variant involves the use of pairs of short synthetic DNA probes fluorescently labeled, containing a “stuffer” to give the pair a unique length in case of multiplexing. The fluorescence peak intensity of each sample amplicon can be compared with the fluorescence peak intensities of a control sample, giving information about copy number variations of specific genomic regions.
However, NGS (Next-Generation Sequencing) can also be used in CNVs detection. In the paper of the month, the authors present an NGS-based approach coupled with confirmatory MLPA for CNVs detection in a patient presenting a high LDL blood level and familial history of heart disease. Thanks to this molecular approach, they identified a novel LDLR large deletion including exons 4-18, leading to the loss of most of the functional domains of the protein. The use of NGS bioinformatics enabled them to bring precision about the breakpoint site and the underlying molecular mechanism.
Our FH panel is an NGS-based kit allowing the characterization of 9 genes involved in FH and to identify FH polygenic SNPs and SNPs for the prediction of statin response, offering an easy-to-use tool for both FH diagnostic and prediction of the therapeutic path. This kit could reduce the cost of genetic testing in FH diagnosis by deleting the cost of MLPA and is relevant for laboratories that don’t have the necessary resources and time to establish a dedicated MLPA workflow for the CNVs’ detection.
(1) Bilen, O., Pokharel, Y., & Ballantyne, C. M. (2015). Genetic Testing in Hyperlipidemia. Cardiology Clinics, 33(2), 267–275.
https://doi.org/10.1016/j.ccl.2015.02.006
(2) Pinal-Fernandez, I., Casal-Dominguez, M., & Mammen, A. L. (2018). Statins : pros and cons. Medicina Clínica, 150(10), 398–402.
https://doi.org/10.1016/j.medcli.2017.11.030
Concolino, P.; De Paolis, E.; Moffa, S.; Onori, M.E.; Soldovieri, L.; Ricciardi Tenore, C.; De Bonis, M.; Rabacchi, C.; Santonocito, C.; Rinelli, M.; et al. Identification and Molecular Characterization of a Novel Large-Scale Variant (Exons 4_18 Loss) in the LDLR Gene as a Cause of Familial Hypercholesterolaemia in an Italian Family. Genes 2023, 14, 1275. https://doi.org/10.3390/genes14061275